HEALTHCARE INFO
CONTENTS:
Records commonly include personal identification information, exam findings, allergies and drug sensitivities, hospitalizations, surgeries, prescribed medications, clinical tests, pregnancy history, test results, health history, and progress notes.
COMMONLY USED SYNONYMS:
medical record, electronic health record (EHR), electronic medical record (EMR), physical data entry electronic medical record (PDE-EMR), health record, medical chart
DOCUMENT TYPES:
- Identification and Admission Documentation
- Admission Record/Facesheet
- Pre-admission Screening (PASARR)
- Admission Consent Permanent
- Admission Agreement
- History and Hospital Records
- Hospital Discharge Summary
- Hospital Transfer Form
- Immunization Records
- Advance Directives / Legal Documents
- Living Will
- Clinical Assessments
- Nursing Assessments
- Wound and Skin Assessments
- Pain Assessment
- Care Plan
- Physicians Orders
- Fax Orders
- Annual Exams
- Medication, treatment, and other Flow Sheets
- Vital Sign Record
- Weights Record
- Intake and Output Records
- Lab, X-Rays, and Special Reports
- Social Service, Dietary (Nutrition Services), and Activities (Therapeutic Recreation)
- Filing and Retrieval
GUIDELINES FOR HEALTH INFORMATION RECORDS SYSTEMS:
It is critical that each medical facility have a formalized system for the maintenance and organization of their medical records. All records should be consistently organized and readily accessible. The guidelines below offer a baseline for the systems that should be in place for maintaining the records systems in a facility.
MAINTENANCE OF THE MEDICAL RECORD
It is important that active and overflow records are maintained in a consistent, organized manner. Records are to have an established order of filing that is followed. All records (overflow records, records on the nursing station, and discharge records) should be readily accessible, kept in an organized chart order, filed in an easily retrievable fashion, and retained in folders or chart holders adequate in size for the volume of the record. The folders and chart holders should be kept clean, neat, and orderly.
IDENTIFICATION (NAME AND NUMBER) ON PAGES OF THE MEDICAL RECORD
Legally, each page or individual document in a medical record should contain identification information including at least patient name and medical record number. If the facility uses labels or label paper, patient information should be included on the label. The patient name and number should be placed on both sides of a document because records are often copied and both sides may not be included. Identification information can be written on the records using permanent ink, stamped with an addressograph, or affixed with a label.
FILING AND RETRIEVAL:
The health care organization’s filing systems, policies, and procedures must comply with federal and state regulations to ensure that all health records are well organized and available in a timely manner to all authorized users. Policies and procedures must be in place to provide the prompt, consistent, uniform, and efficient filing of all health records. The system of filing should ensure the safety, security, and accuracy of health care records. The retrieval system should be structured to ensure the safety, security, and accuracy of health records. Measures must be in place to keep track of the location and holders of health records and to follow-up at appropriate intervals on the return of the health records. Procedures must also be in place to identify the health records that need to be converted to a different medium and moved to inactive storage or destroyed. (1)
THE TWO FORMS OF MEDICAL RECORDS:
Medical records, or healthcare records, are generally in two forms – paper and electronic. Each has its limitations. The federal government has mandated that all health care information will be stored electronically. However, there will still be paper-based medical records around for quite some time
PAPER-BASED MEDICAL RECORDS
GENERALLY, ONE OF THREE FORMATS USED:
Source-oriented – like documents are grouped together (i.e. labratory reports, radiology, physician’s progress notes, etc.) Usually filed in reverse chronological order.
Pros: It is easy for individuals doing filing of reports, etc.
Cons: Caregivers have to reference each section by date of occurrence to get a full picture of the patient’s course of treatment.
Problem-oriented – arranged according to problem/occurrence. Each problem/occurrence of the patient is indexed with a unique number. All reports, clinical documentation, progress notes, care plan, and other patient data are identified with this unique number. It is then generally arranged in reverse chronological order sections, each which covers a specific problem/occurrence.
Pros: Caregivers can easily follow patient’s course of treatment and progress.
Cons: Inconsistency of application of the problem numbers.
Integrated – All documentation from various sources is intermingled and follows either chronological or reverse chronological order.
Pros: Easy for caregivers to follow course of patient’s diagnosis and treatment.
Cons: Difficult to compare related information.
SOME LIMITATIONS OF PAPER-BASED MEDICAL RECORDS ARE:
Can only be viewed by one individual at a time, therefore, may be unavailable to other users when needed.
Difficult to update – paper documents must be hand carried to where the chart is located possibly delaying the filing of latest information
Maintaining duplicate copies (backups)expensive, usually cost prohibitive
Always at risk of being misplaced, misfiled, or damaged
ELECTRONIC MEDICAL RECORDS (EMR OR EHR):
Results of the health record evolution. Solves many of problems that affect paper-based medical records.
Pros: EHR systems allow access to information quickly and easily, Provides various levels of access, Multiple users can access at same time, Easier to handle and maintain, Can be copied/backed up to various electronic storage media in a secure location onsite or offsite, and thus protected from damage, loss, and tampering.
Cons: Expensive to implement and maintain, Extensive training required for health care users, Need to redevelop policies and procedures, Process changes required
True EHRs are not just digitized paper records, but rather the capture of data with the capability of retrieval of that data using electronic technology to allow full functional decision support. The system must also protect the security of the patient identifiable information and the integrity of the clinical documentation, as well as, be available for multiple users at the same time. Most healthcare organizations today store the digital version of the paper records. Experts say this is the first step to true EHRs.
HEALTHCARE RECORD NUMBERING SYSTEMS:
There are several numbering systems used for medical records. The most common are serial, unit, and serial-unit.
Serial – Each patient is assigned the next number in the series. If the patient is admitted multiple times, each time a new number would be assigned for that admission. A patient would have completely separate records making it difficult to compare information from the different admissions.
Unit – Each patient is assigned a unique number on the first admission, and it is used for each subsequent admission. All records are filed together saving cost and labor. However, during the admission process, the facility’s master list must be checked to make sure the patient does not already have a number.
Serial-unit – Uses both the serial and unit system. In this system, the staff assigns the next number in the series. Any records from previous admissions are retrieved and combined with the current one. When the current admission is complete, all the records are stored under the most recent number.
FILING SYSTEMS:
Alphabetical – Generally used only in small facilities/clinics or single physician offices. In this system the patient record is filed by last name, first name, and middle name. The birth date is commonly used to differentiate between duplicate names.
Numeric – Filed in a numeric sequence. Used in larger facilities that have high patient volume. This system relies on a master patient index that lists the patient’s name and the record number.
THE THREE MOST COMMON NUMERIC TYPES ARE:
Straight numeric filing – Arranged consecutively in ascending order.
Terminal-digit – Last digit or group of digits determine file placement. Typically a three-part number made up of two-digit pairs.
Alphanumeric – A combination of alphabetic letters and numbers are used. Commonly, the first two letters of a patient’s last name plus a number.
Purges are generally done by year using the discharge or “last seen” date.
STORAGE SYSTEMS:
PAPER-BASED
Lateral file cabinets – Used in smaller facilities, but do not make good useage of expensive floor space. While better than vertical file cabinets, they still require additional footprint space. There are automatic lektreiver systems similar to vertical file cabinets where shelves are on a rotating drum and rotate to access the various shelves.
Fixed open shelf systems – Most common system. These systems consist of open racking with space allowed for aiseles to access the files. The folders have side tabs for easy retrieval.
High density mobile systems – These are also called compressible. They are like the fixed open shelf systems except that the shelves are on tracks in the floor and can be moved and opened as necessary to access the records. These are good for high patient volume and where floor space is at a premium.
MICROFILM BASED
Microfilming paper records will reduce the amount of storage space substantially. It is good for inactive or infrequently used medical records. However, not good for active or frequently used records.
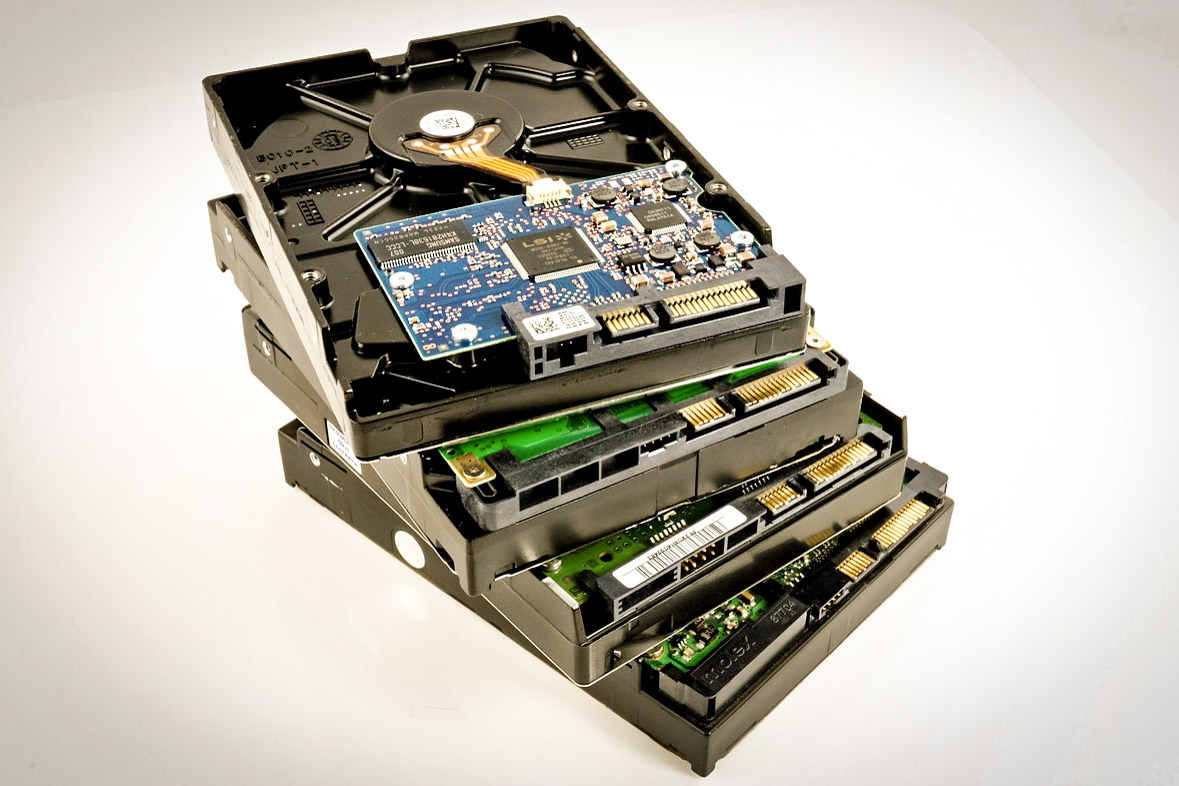
IMAGE-BASED
Source documents are scanned to disk (optical or hard drives on servers) as images. Access is easy and fast, and it is available to multiple users at the same time. These systems are capable of scanning thousands of images in a day. The images can then be loaded into EHR systems. (4)
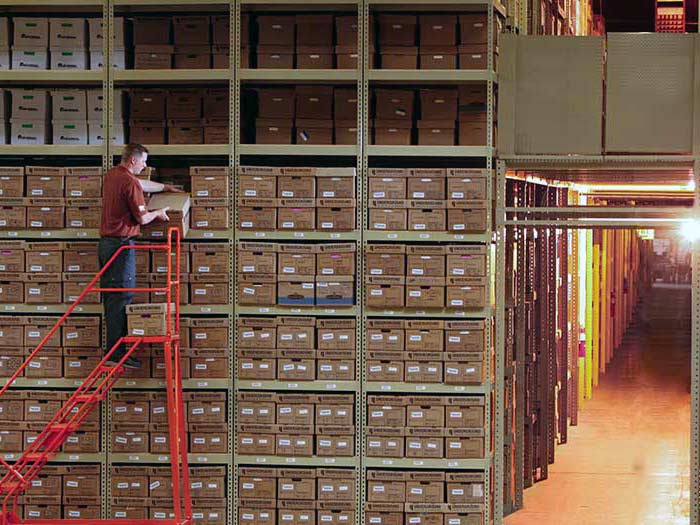
STORAGE BOXES:
When it becomes necessary to move inactive medical records to offsite storage, storage boxes are used. Boxes used should be of adequate quality and durability for record storage purposes. It is best to stack no more than three boxes high to maintain the integrity of the boxes. Boxes should be placed on shelves to facilitate easy retrieval. They should not be placed on the floor. Boxes should be at least 6″ above the floor and 18″ below sprinkler heads.
MAINTAINING A RECORD CHECK-OUT SYSTEM:
One of the most important physical security measures that must be in place at every medical facility is a record sign-out system for all medical records. Not only should these systems be in place, but they must be enforced to be effective. Health information staff should monitor the sign-out practices and assure that records are returned in a timely manner.
Active Records – Outguides or a sign-out system must be in place. Charts should not leave the storage location without being signed out. Outguides work well because they are placed where the chart was removed. The authorized person who took the record must be identified along with the date and location.
Inactive Records – Regardless of where inactive records are located in the facility, there must be a sign-out process to identify when a record has been removed, who took the record. and where it is located.
CONFIDENTIALITY AND RELEASE OF INFORMATION:
HIM (Health Information Management) Standard
The medium in which resident-identifiable data and health care information are stored, whether paper based or computer based, is the property of the health care organization and is maintained to serve the resident, the health care professional, and the health care organization in accordance with the legal, accrediting, licensing, regulatory, and ethical standards.
Medical records and health care documents, regardless of the medium in which they are stored, belong to the patient and are protected accordingly.
Confidentiality policies and procedures specify that patient-identifiable data and health care information are used within the health care organization only for the purpose for which the data and information were collected.
Sources Cited:
(1) “Off-site Data Protection.” Wikipedia, The Free Encyclopedia. 17 Sep 2006, 23:51 UTC. Wikimedia Foundation, Inc. 29 Sep 2006
LEARN MORE
(2) “Magnetic Tape Summary” PCMAG.COM 29 Sep 2006, 08:31 UTC. The Computer Language Company, Inc. 29 Sep 2006
LEARN MORE
(3) “IBM TotalStorage Enterprise Tape System 3590 Operator’s Guide” Sep 2004. International Business Machines Corporation.
LEARN MORE
(4) “Backup rotation scheme.” Wikipedia, The Free Encyclopedia. 12 Jul 2006, 15:20 UTC. Wikimedia Foundation, Inc. 29 Sep 2006
LEARN MORE